Investigator Spotlight: September 2015
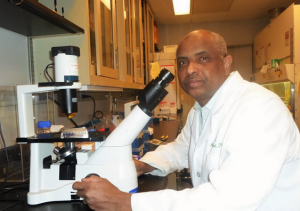
Abdu Hamad, PhD
Dr. Hamad is an associate professor at Johns Hopkins University School of Medicine. Dr. Hamad joined nPOD in 2011.
-
Tell us about your education and background – where are you from, where did you go to school?
I am originally from Sudan and am a veterinarian by training. After graduating from the veterinary school at the University of Khartoum, I completed a masters in Microbiology and then moved to the US where I completed a Ph.D. in Immunology under the supervision of John Kappler at the National Jewish Center in Denver. After that I moved to Baltimore where I did my postdoctoral training under the supervision of Dr. Drew Pardoll at Johns Hopkins University School of Medicine.
- Where do you currently work and what is your position? What does a “day in the life” look like for you?
I am currently an associate professor of Pathology and Medicine at Johns Hopkins University School of Medicine in Baltimore, Maryland. - Why diabetes? How did you get involved in diabetes and/or what made you want to work in diabetes research?
I got involved in the study of autoimmune diabetes by serendipity. This happened towards the end of my postdoctoral training when I became interested in double negative (DN) T cells while studying MCC-specific TCR transgenic T cells stimulated magnetic beads coated with anti-CD3/CD28 beads. This led me to study DN T cells that cause lymphoproliferation in mice bearing homozygous loss-of-function mutations in FasL (gld mice) or Fas (lpr mice). Despite massive DN T cell lymphoproliferation, NOD mice bearing homozygous gld or lpr mutations become completely protected from developing autoimmune diabetes. Since the Fas pathway is not essential for the host defense, we have been invested in understanding how inactivating FasL prevents autoimmune diabetes and the relevance of this preclinical phenomenon to the human T1D. We have made significant progress in deciphering the underlying mechanism and dissociating the lymphoproliferation from the protective effect of the gld mutation (discussed below) and gaining insights into the underling mechanisms. We hope that our research in this area will lay the groundwork for establishing FasL as a safer therapeutic target. In regards to what made me want to work in diabetes research, it is the nature of the disease and the fact that it affects children, including infants, and that it has no cure and never goes away. Indeed, T1D puts a huge burden and strain on lifestyles of affected children and their families. In addition, parents of at risk children are constantly worried that their children might become diabetic. Thus, any contribution that we make as investigators towards ameliorating the risk of T1D will be highly rewarding. - Tell us about your research.
T cells are the orchestrators of immune responses and arguably represent the most important immune cell type. T cells detect and destroy invading pathogens without harming self-tissues. However, not all T cells are good; some are autoreactive in the sense that they mistakenly recognize self-tissues as foreign entities and work to destroy them. In individuals not prone to autoimmunity, multiple mechanisms serve either to eliminate or keep rogue T cells in check. Additionally, tight surveillance is conducted by specialized subtypes of lymphocytes that we refer to as regulatory cells. In many at-risk individuals, these protective mechanisms eventually fail, leading to the freeing of rogue T cells that proceed to attack and destroy insulin-producing beta cells and necessitate insulin replacement therapy. Thus, a major focus of T1D researchers is directed towards devising strategies to suppress or eliminate rogue T cells without harming productive T cells. The challenge in achieving this goal is illuminated by the fact that productive and rogue T cells utilize similar mechanisms to survive, proliferate and attack their targets, whether invading pathogens or self-tissues. These similarities make it difficult to find a method to safely pinpoint and remove rogue T cells with minimal damage to the productive T cells that are required to maintain a strong host defense against infections and cancers. Identifying such strategies is the challenge that keeps most of us awake at night. To overcome this problem, our research is focused on the unorthodox approach of inhibiting the Fas death pathway. This strategy is based on the experiment-in-nature that spontaneous loss-of-function mutations in the Fas pathway completely protect the non-obese diabetic (NOD) mice from developing diabetes without causing immunosuppression. However, it has been unclear how blocking the Fas pathway prevents autoimmune diabetes. Our research indicates that rogue B lymphocytes erroneously use this lethal system to kill regulatory cells responsible for suppressing rogue T cells. This takes the brake off rogue T cells and allows them to proceed to infiltrate pancreatic islets and destroy insulin-producing beta cells. Our research in the NOD mouse model shows that this problem is fixable by partially inactivating the Fas death pathway to protect regulatory B cells from deletion and maintaining their role in putting the brake on rogue T cells. The ability of a FasL-neutralizing monoclonal antibody called MFL4 mAb to protect NOD mice from diabetes and restoring regulatory B cells raises hope that this discovery can potentially be translated into a treatment.

Thus, besides continuing our fundamental analysis in NOD mice, we are currently using samples from patients and healthy controls, including samples provided by JDRF/nPOD to assess the relevance of our preclinical findings. Our preliminary findings are highly encouraging and suggestive that similar defects in the Fas pathway may be found in diabetes development in humans as well. If proved true, blocking the Fas pathway with biologics could offer a safer strategy to protect high risk individuals from developing diabetes. More information can be found at our website: http://pathology.jhu.edu/hamad/index.cfm.
- What are your thoughts on the progress being made in T1D research as a whole?
Luckily, through global efforts spearheaded by JDRF, new information is being acquired around the clock on disease pathogenesis using the NOD mouse model. The collected information has led to many immunomodulating strategies that prevent the disease in NOD mice. However, translation of these modalities into immunotherapies has been challenging and efficacy was much less than expected. Hence, the establishment of nPOD was a major strategic milestone in the field because it provides a path for studying and understanding the disease process in humans. Before nPOD, peripheral blood was the only human sample available for researchers. Now, researchers can study the disease process in the pancreas, which is critical for accelerating the development of immunotherapy for T1D. - Why is diabetes research so important?
There are several reasons. First and foremost is that T1D is a chronic disease that strikes early in life (including during infancy) and never goes away. It puts a lot of strain on patients and their families. Second, T1D incidence is increasing worldwide at alarming rate: this has serious long term complications. Therefore, any contribution to finding a cure for the disease will be highly rewarding. There are increasing hopes that the development of modalities that will protect those at risk and perhaps reverse or slow T1D progression is not that far away. - Do you have anything extra you would like to share? Is there anyone to thank or acknowledge?
My Ph.D. mentor, Dr. John Kappler, his wife and lifelong scientific collaborator, Dr. Pippa Marrack for accepting me in their lab and giving me the training that has shaped my academic career and for their ongoing support. I am also thankful for my postdoctoral supervisors, Dr. Drew Pardoll and Dr. Jonathan Schneck, for their continuous support. Funding from JDRF early on in my career played a critical role in keeping me afloat and gave me the opportunity to focus my research program on diabetes, and NIH funding allows us to continue and sustain our research and momentum. I am also grateful for nPOD for giving us the resources to assess the relevance of our preclinical findings to T1D. And of course to my wife Amal and my three kids for their support, and the joy they bring every day to my life. - When you’re not working, what do you like to do for fun?
I love going to the gym, which is highly refreshing, especially after a long working day. I also love cooking, especially traditional Sudanese food.